
Xiongfei Liu, MD
Cataract and Glaucoma Specialist
Treatment of glaucoma consists of medical and surgical therapies. While surgical therapy is gaining traction (especially in the area of MIGS), medical therapy remains the cornerstone of treatment algorithms. Therefore, today’s topic will focus on the different options of medical therapy and their side effects, as well as a sneak, peek of what we might have in the future.
For most ophthalmologists in the US, the first line of medical therapy is the eyedrop latanoprost, which is a class of prostaglandin that is very powerful in lowering eye pressure. Its main mechanism is to enhance the outflow pathway, which is effective for 24 hours. Its regimen is once a day, which is very simple to keep track of. It has several cousins in its class, which includes bimatoprost (Lumigan as a brand), travoprost, and tafluprost. The most common side effects consist of red-eye, irritation, lengthening, and thickening of the eyelashes (which might be a good thing). Other not so common side effects include fat atrophy around the eye socket with steepening of the superior eyelid crease, as well as gradual changes of iris color (a reason not to use latanoprost in just one eye). Prostaglandin is the only class of medication where if you are not responsive to, let’s say latanoprost, then your doctor will switch you to either bimatoprost or travaprost rather than a new class of medication.
The second line of medical therapy is undergoing a paradigm shift these days. Before Rhopressa came onto the market, timolol was most likely the go-to medication. It is effective and is dosed at once a day in the morning to prevent nighttime pressure dip that can affect the visual field in the long run. Timolol was the first-line of therapy prior to latanoprost coming to market in 1998. Timolol, however, can have systemic side effects if absorbed systemically. These effects include slowing of the heartbeat, low blood pressure, as well as triggering a tightening of the chest that is of particular concern for someone with asthma and COPD. On a side note, timolol or its systemic cousin propranolol is often used by individuals who have stage fright and use the medication to calm their nerves.
Dorzolamide and brinzolamide round out the next line of therapy because dorzolamide can simply combine with timolol in a single eye drop called Cosopt. The dosage for Cosopt is twice a day. For dorzolamide, it is usually well-tolerated as a topical therapy. It has a 24-hour effect. Therefore, if a patient has normal-tension glaucoma, I would probably put dorzolamide as a second line of therapy after latanoprost for a 24-hour sustained effect. Dorzolamide’s cousin, acetazolamide, is a systemic medication that can be taken as a pill either two to four times a day, with different concentrations. The pill is the most effective out of all the medical therapies, but it can exacerbate kidney function if the patient has a history of kidney stones, and is therefore not suited for someone with compromised kidney function. Furthermore, one can experience tingling around the fingertips, nausea, and general weakness. It is not a medication that I would put someone on for the long haul.
Brimonidine makes up the last line of the traditional eyedrops. It is effective and is dosed two to three times a day. Unfortunately, it is often poorly tolerated due to its propensity to cause ocular side effects. These include high rates of eye redness and allergy changes. Furthermore, patients can experience dry mouth and drowsiness with decreased energy.

In the last few years, a couple of new eye drops have come onto the market. Rhopressa is one of them. It works by increasing the traditional outflow pathway, as well as lowering the episcleral eye pressure. Episcleral eye pressure determines the lowest ocular pressure that the eye can sustain at a physiological state. By lowering episcleral eye pressure, Rhopressa has the potential to lower one’s ocular pressure to the low teens and in rare cases, even the single digits. Rhopressa also works well in tandem with latanoprost, and their combination eye drop is called Rocklatan, which is dosed once per day. Side effects of Rhopressa include eye redness and tiny conjunctiva bleeding, as well as a spiderly pattern on one’s cornea that rarely affects eyesight at all. Rhopressa is very nice medication, and I’ve started to use it as a second-line therapy to combine with latanoprost. The only downside is from insurance, as at times one needs to go through the loop to get the patient on Rhopressa or Rocklatan.
The other new kid on the block is Vyzulta. The dosage is once a day, and it works in multiple ways including decreasing ocular fluid production as well as increasing fluid outflow. Similar to Rhopressa, it can cause eye redness. Overall, it is a great medication that can serve as a second-line therapy as well (the catch is that its effect overlaps with latanoprost, so its effect might not be as strong as a second-line therapy versus first-line).
SIDE EFFECTS AND WHAT WE CAN DO ABOUT IT
Now that we have gone over the different types of medical therapy, I believe that a lot of patients are more or less not perfectly satisfied with their current eyedrops. These eyedrops either make their eyes feel irritated, red, or both. The most common reason for these side effects is the preservatives inside the medication. The preservatives are necessary to prevent microbial growth while the eye drop is being stored. However, the antibiotic activity can also irritate the surface lining of the eye as collateral damage.
Several initiatives have been done to minimize the side effects of these preservatives. The first one is a combination drop like Cosopt. It is dosed twice a day, and each drop has a similar amount of preservatives as either timolol or dorzolamide. Therefore, you get the pressure-lowering effects of two eyedrops for the cost of one eyedrop’s irritation from preservatives. Another way to combat eye irritation and related allergies is to instill artificial tears that can be dosed at four times a day if needed. One can either put them a few minutes before or after the glaucoma eye drops to minimize the irritation. Last but not the least, one can use a preservative-free glaucoma eye drop, or drop with a milder form of preservatives. These medications include preservative-free Cosopt, Alphagan P, Travatan Z, etc. The downside is that these drops are often more expensive. From an insurance standpoint, prior authorization sometimes has to be filed detailing the previously failed attempt of eye drops with preservatives. Nevertheless, these drops are effective at decreasing eye irritations.
In my clinic, after we have tried preservative-free eye drops, the next line of treatment would be to try dry eye medications like Restasis twice a day or Xiidra. These eye drops have been shown to improve the ocular surface which is often marred by glaucoma eye drops. If the effects are still lacking, or patients are scheduled for glaucoma surgery in the near future where the ocular surface needs to be improved, then I would place them on a two-week trial of low dose steroid (lotemax) eye drops to improve the situation. If all these approaches still fail, then I will consult with the patients face to face regarding their opinions on glaucoma surgery, since surgery can lower ocular pressure and spare them the misery from some of the eye drops.
WHAT WE ARE LOOKING FORWARD TO
Given the burden associated with preservatives, innovative minds have worked on ways to provide sustained medication release with a minimal touch of preservatives. One quick example is Durysta. Durysta is a biodegradable implant that is injected into the anterior chamber of the eye. 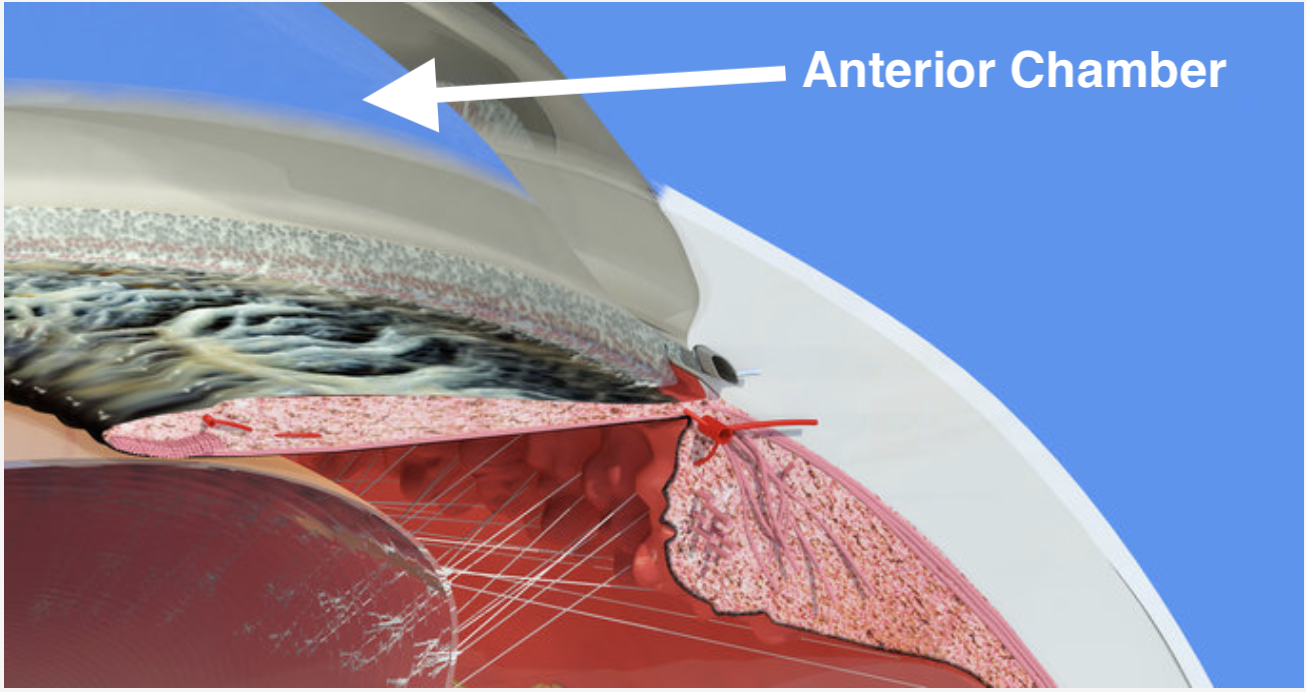
It consists of bimatoprost that can slowly and sustainably release itself over the course of three months. Currently, it is only approved for one-time use. But imagine not needing to use an eyedrop for three months by having the Durysta implant in each eye (the injection process is often done in the clinic very quickly), which saves effort, money, and inconvenience from eye irritation. The technology will only improve in the future, and there will likely be other implants from other medication classes that could potentially be approved for more than one-time use years from now. Another exciting medication delivery system that is underway is iDose. It is still in phase 3 trials right now, but it has the potential to be a game-changer in the way we look at medical therapy in the future. I surely look forward to it when it will be on the market, and I will explain more about it in the coming blogs. Stay tuned!











